Abstract
BACKGROUND
Hypogammaglobulinemia (HYPO) is a typical feature of chronic lymphocytic leukemia (CLL), with an incidence of 20-60% at diagnosis and a relationship with infections occurrence. Predictive and prognostic factors are well known (IGHV, del11q, del17p, TP53); CLL-IPI score including age, clinical stage, beta2microglobulin, IGHV and deletion 17p and/or TP53 mutation has been recently validated. It identifies 4 risk groups with significantly different time to first treatment (TTFT) and overall survival (OS). Prognostic significance of HYPO at diagnosis has not been extensively evaluated in terms of OS and TTFT. Only IgG serum levels have been reported to be associated with TTFT but no data are available on other immunoglobulin classes (Ig).
AIM To evaluate the impact of HYPO and single Ig classes on TTFT in a retrospective cohort of CLL patients and to assess the relationship between HYPO and CLL-IPI.
METHODS
We retrospectively evaluated 698 consecutive CLL patients diagnosed at our Institution from 1983 till 2016. Data from laboratory, biological analysis and clinical stage were collected. We also evaluated immunoglobulin (Ig) status (i.e. IgG, IgM and IgA) at diagnosis and calculated CLL-IPI. HYPO was defined basing on our laboratory cut-offs (IgA 70 mg/dl, IgG 700 mg/dl, IgM 40 mg/dl). However, as no recognized prognostic/predictive Ig cut off has been reported to date, we aimed to identify a prognostic threshold for each Ig class.
RESULTS
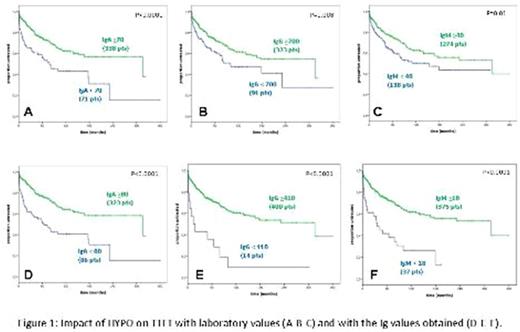
From 698 patients assessed, 410 cases were evaluable for Ig values at diagnosis. IgA levels were lower than 70 mg/dl in 17,4%, IgG lower than 700 mg/dl in 22,2%, and IgM lower 40 mg/dl in 33.7%. Forty-six percent of patients presented deficit of at least one Ig class, while 7.8% of patients had all Ig low. Each Ig deficit was related with a shorter TTFT with the following hazard ratios (HRs): 2.09 (1.45-3.03) for IgA (P<0.0001), 1.58 (1.10-2.27) for IgG (P=0.008) and 1.52 (1.09-2.13) for IgM (P=0.01) (Figure 1, A-B-C). However, only IgA deficit maintains statistical significance in multivariate analysis [HR 1.59 (1.08-2.35)].
A prognostic threshold for each Ig class was identified maximizing the differences in TTFT and the following values were obtained: 80 mg/dl for IgA, 410 mg/dl for IgG and 18 mg/dl for IgM (Figure 1, D-E-F).
Considering CLL-IPI, 186 patients presented IPI 0-1, 99 had IPI 2-3, 32 patients IPI 4-6, and 12 patients had IPI 7-10. Even in our series, CLL-IPI separated four risk groups with different TTFT and OS, suggesting that our cohort may be suitable to evaluate new prognostic factors. As regards the relationship between HYPO and CLL-IPI, we observed a correlation with IgA levels, using our laboratory cut-off. Moreover, we found a relationship among CLL-IPI and both IgA and IgM values, when using the newly validated Ig cut-off. Finally, CLL-IPI was a stronger prognostic factor for TTFT than HYPO in our analysis. However, the addition of IgA deficit to CLL-IPI appears to further improve CLL prognostication.
CONCLUSION
Our analysis supports the impact of HYPO on CLL prognosis. Although CLL-IPI has a stronger prognostic value for TTFT compared to HYPO, the inclusion of IgA deficit appears to further improve accuracy on CLL prognostication.
Barcellini: Alexion: Honoraria; Agios: Honoraria, Research Funding; Novartis: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.